EURenOmics Project Summary Year 3
Summary description of project context and objectives
Rare kidney diseases impact markedly on the life expectancy and quality of life of affected individuals. The current diagnostic and therapeutic management of rare kidney diseases is highly unsatisfactory. We are typically unable to explain the genetic or molecular abnormality underlying the disease phenotype, to predict the individual risk and rate of disease progression, or to quantitate the risk of relatives to develop the same disorder. Even in patients with known genetic causes, individual risk prediction is limited by considerable phenotypic variability. Molecular disease and progression risk markers are lacking. Effective therapies are largely unavailable; the lack of suitable disease models is a major barrier to therapeutics development.
Kidney diseases are well suited to high-throughput research due to the opportunity to examine molecular events in the end organ that is manifesting the disease: kidney biopsy, a standard diagnostic procedure, provides a unique opportunity to study intrarenal biological processes ex vivo using transcriptomic, proteomic and morphological approaches. Urine is a readily available non-invasive bioresource to study molecular readouts directly derived from the organ of interest, the kidney. Amniotic fluid, the fetal urine, allows prenatal epigenetic, proteomic and metabolomic profiling in the context of renal maldevelopment. Recent technological progress in exosome isolation from urine and amniotic fluid even has created the opportunity to study non-invasively cellular biomaterials originating from the diseased tissues.
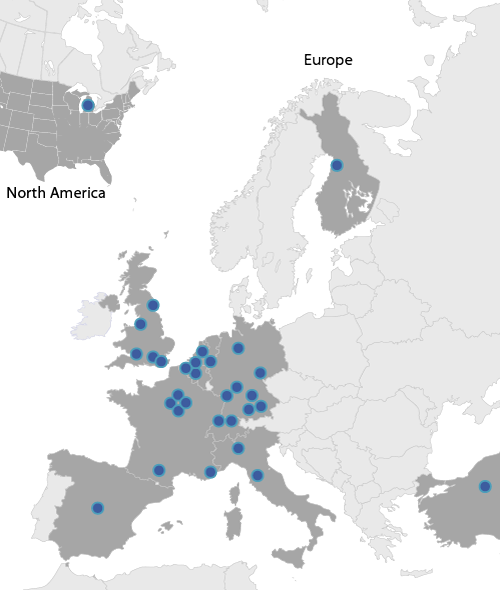
EURenOmics has prioritized five disease groups based on their urgent need and significant potential for diagnostic and therapeutic progress: Steroid-resistant nephrotic syndrome (SRNS), membranous nephropathy (MN), tubulopathies, complement disorders and malformations of the kidney and urinary tract (CAKUT). The consortium has access to a unique assembly of large existing patient cohorts and biorepositories, encompassing more than 15,000 patients with >10,000 DNA, >3,000 serum, 2,000 urine, 500 amniotic fluid and 3,000 kidney biopsy specimens. Some 30 academic and industry partners have joined EURenOmics to apply a wide range of high-throughput technologies, innovative systems biology approaches and a plethora of in vitro, ex vivo and in vivo models to study disease mechanisms and explore novel therapeutic approaches.
Initial research efforts focus on methodological standardization, involving procedures for acquisition and processing of biospecimens but also the construction of an integrated phenome database for uniform clinical phenotyping. The next objective is to search for new genes causing, modifying or predisposing to individual disease phenotypes. Screening strategies encompass next-generation sequencing of known genes, regulatory regions, exomes and whole genomes, application of cutting-edge bioinformatic tools for data mining, filtering and gene network analysis, and extensive genotype-phenotype analyses utilizing standardized phenotypic information. Novel epitopes/antigens and antibodies are searched systematically in those disorders in which an auto-immune pathology is suspected. The protein products of the newly identified gene variants, as well as the mechanisms of auto-antibody formation, are functionally characterized by an array of in vitro, ex vivo and in vivo technologies. Multi-level -omics profiling (mRNA, miRNA, peptidome/proteome, metabolome) in body fluids and renal tissues is performed to identify unique molecular disease signatures (deep phenotyping), develop a prognostically indicative new ontology of rare kidney diseases, discover molecular markers and pathways associated with disease activity and progression, and develop diagnostic tools and biomarkers. Finally, in vitro and in vivo models will be developed that allow high-throughput screening of compound libraries for novel therapeutic agents reversing or attenuating disease phenotypes.
Work performed since the beginning of the project and the main results achieved so far
Numerous novel methodologies including groundbreaking diagnostic and disease activity assays (e.g. an endothelial cell assay for therapeutic monitoring in complement diseases) have been established. A central ‘phenome’ database will integrate clinical information from all patient registries. A unique kidney-focused bioinformatic analysis pipeline containing information from 32 transcriptomic and proteomic datasets is now functional.
Exome sequencing has been performed in 120 families (WP2: n=39, WP4: n=17, WP5: n=28, WP6: n=36). These efforts led to the discovery of 4 novel SRNS genes, 2 tubulopathy genes, 3 complement disease genes, 1 gene causing CAKUT, and 7 new genomic rearrangements in complement disorders. Moreover, numerous candidate disease genes are undergoing functional characterization. Moreover, causative mutations in known genes were found in 8 SRNS, 5 tubulopathy, 10 complement disease and 3 CAKUT families.
In parallel, targeted NG sequencing assays capturing all known genes within each disease group have been developed for glomerular (34 genes), tubular, (39 genes) and complement diseases (29 genes). After careful assay validation, panel screening is being performed on all archived samples and incident patients. So far, panel sequencing has been applied in 614 SRNS, 327 tubulopathy and 108 (atypical hemolytic uremic syndrome (aHUS) cases. Disease causing mutations were identified in 21% of the SRNS and 57% of the tubulopathy cohorts, and correctly recovered in 95/108 aHUS patients. The tubulopathy kit has been submitted for use as the national reference NGS diagnostic tool in the UK.
The rapid advances in gene diagnostics enable the Consortium to perform detailed genotype-phenotype association studies in sizeable cohorts of genetically classified patients (e.g., WT1 and ADCK4 glomerulopathy, Dent’s disease, familial hypercalcemic hypocalciuria, renal Fanconi syndrome, autosomal dominant tubulointerstitial kidney diseases (ATKD), C3-associated aHUS), and decipher the functional impact of key mutations in individual disease genes.
Fundamental progress in the understanding of genetic disease penetrance was achieved. In NPHS2 glomerulopathy, the expression of a phenotype in compound heterozygous patients was found to depend on the nature of the combining mutations. This discovery is the first description of mutation-dependent recessive inheritance. Enrichment of rare variants in renal developmental and complement genes is emerging as another important determinant of disease predisposition.
Major progress was also made concerning the molecular mechanisms of auto-immune disease. The B cell epitope in PLA2R, the target of autoantibodies in MN, has been identified. Academic and industry partners jointly identified the HLA peptidome, paving the way for unbiased identification of immune response targets in autoimmune diseases. In CFH-antibody mediated aHUS autoantibody formation was found to emerge from deficient B-cell regulation by genetic CFHR3 deficiency, demonstrating a mechanistic link between genetic disease and autoimmunity.
Notably, our studies in rare nephropathies emerge to provide clues as to general risk factors for kidney disease development and progression; e.g., variants in the ATKD gene UMOD, predispose to chronic kidney disease and hypertension, and abnormalities in the complement gene CFHR1 affect the risk and progression of the common IgA nephropathy.
In the search for new therapies for rare kidney diseases, a randomized clinical trial has established the safety and superior efficacy of the anti-B-cell antibody rituximab in MN. The discovery of mutations in mitochondrial genes potentially responsive to oral CoQ10 supplementation may herald effective prevention of renal failure in a significant subset of hereditary SRNS. Finally, there is early progress in model devleopment for compound screening including cell-based assays as well as animal models for SRNS, tubulopathies and complement disorders.
The expected final results and their potential impact and use (including the socio-economic impact and the wider societal implications of the project so far)
The research results expected from EURenOmics will have substantial impact on diagnostic management, risk assignment and preventative and therapeutic strategies in patients with rare kidney diseases, with potential implications also for patients with common kidney and other diseases and the society at large.
Comprehensive exome sequencing of large patient cohorts is profoundly advancing the state of knowledge by unraveling the as yet unknown monogenic and complex genetic causes underlying the diseases of interest. The newly discovered genes are continuously included in the targeted next-generation sequencing (NGS) gene arrays developed by the partners. The advent of these NGS panels is considered a major breakthrough as it will render the current sequencing technology with its high cost and time demands obsolete and will bring rapid and complete genetic diagnostics into routine clinical practice. For those patients in whom a genetic diagnosis cannot be established, we seek to develop disease-specific RNA, proteome and metabolome profiles and novel auto-antibody assays in the course of the project.
The availability of such rapid diagnostic tests will constitute a big step towards personalized medicine. The need for invasive kidney biopsies will be greatly reduced or eliminated. Exposure to ineffective, potentially toxic and costly medications can be avoided and replaced by rational, risk-adapted therapies tailored to the molecular basis of mechanistically defined disease entities. The recent development of a sensitive and specific bioassay that allows to monitor therapeutic complement blockade and prevent both hazardous under- and costly overtreatment with the C5 inhibitor eculizumab in complement disorders exemplifies the remarkable health and socio-economic impact of the Consortium’s activities.
In addition to the expected diagnostic progress, the anticipated identification of genetic disease causes and risk factors as well as prognostic biomarkers should greatly facilitate individual risk assignment regarding disease occurrence, progression, complications and post-transplant recurrence compared to the currently used clinical, histopathological or imaging criteria. The efficiency of genetic counselling to families with inherited disorders will be much improved, alleviating their psychological burden and distress. Also, accurate risk assignment will form a basis for the development of early intervention and secondary prevention protocols.
Moreover, the partners have started developing in vitro and in vivo disease models aimed to discover novel therapeutics including alternatives to existing superexpensive drugs, and to allow a more rational, calculated use of already available agents. Our preliminary results and ongoing research efforts with respect to in vitro and in vivo model development, the repurposed use of approved pharmaceutical agents to attenuate hereditary glomerulopathies and the development of a novel complement blocking monoclonal antibody look promising and will contribute to the IRDiRC goal of establishing new therapies for a significant number of rare diseases by 2020.
Finally, EURenOmics seeks to generate clinical and socioeconomic impact beyond the field of rare kidney disease. The study of the genetic abnormalities and molecular mechanisms underlying the selected disorders is hoped to produce insights into general mechanisms of kidney disease progression and even universal risk factors relevant to the general population. Our identification of a mechanism by which genetic variation of a kidney-specific protein involved in a rare kidney disorder predisposes to chronic kidney disease and hypertension impressively exemplifies the far reaching potential of rare kidney disease research.